Intrauterine devices (IUDs) are a popular and highly effective form of long-term birth control used by millions of women worldwide. However, one of the most common concerns women have when considering an IUD is the potential pain or discomfort during and after insertion. Fortunately, guidelines and recommendations, including those provided by the CDC (Centers for Disease Control and Prevention), offer advice on IUD insertion pain management to help make the procedure as comfortable as possible.
This blog will cover everything you need to know about CDC IUD insertion pain management, including the types of IUDs, what to expect during the insertion process, pain management options, and frequently asked questions about the procedure.
What is an IUD?
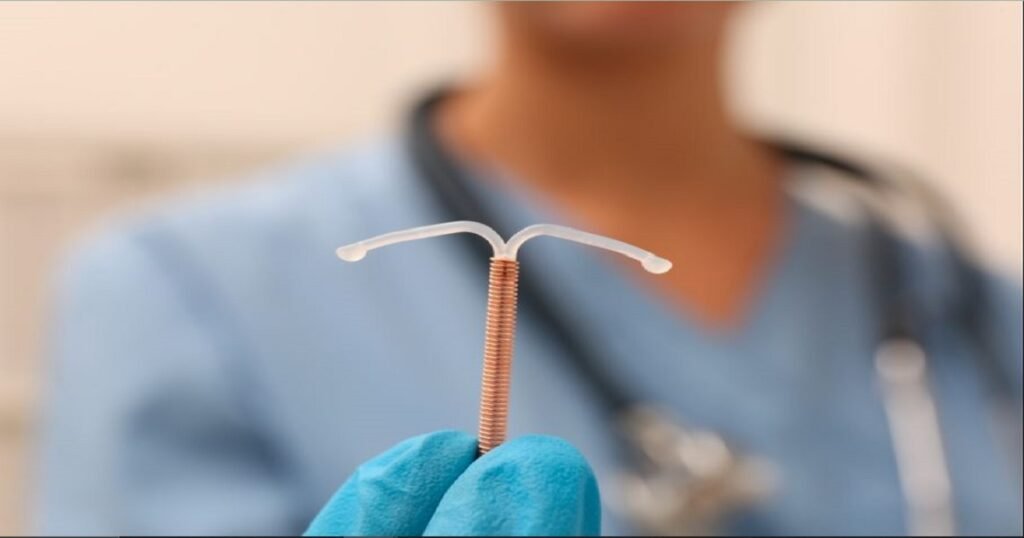
An IUD is a small, T-shaped device that is inserted into the uterus to prevent pregnancy. There are two main types of IUDs:
- Hormonal IUDs: These release small amounts of progestin, a hormone that thickens cervical mucus and prevents sperm from reaching the egg. Hormonal IUDs are typically effective for 3 to 7 years, depending on the brand.
- Copper IUDs: Copper IUDs are non-hormonal and work by creating an inflammatory reaction in the uterus that is toxic to sperm. Copper IUDs can prevent pregnancy for up to 10 years.
Both types of IUDs are over 99% effective at preventing pregnancy, making them one of the most reliable forms of birth control.
What to Expect During IUD Insertion
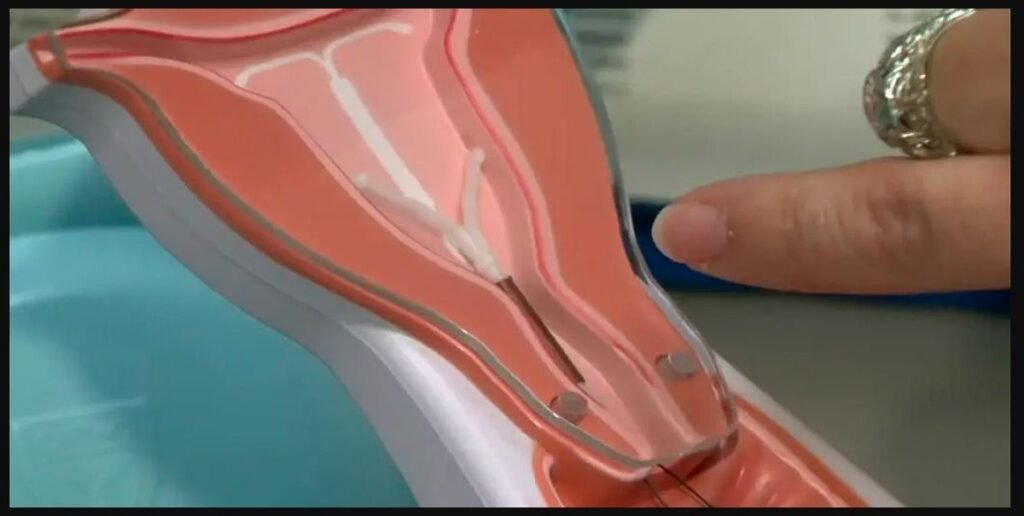
IUD insertion is a quick, in-office procedure that usually takes about 10 to 15 minutes. During the procedure, your healthcare provider will insert a speculum into the vagina, similar to a Pap smear, and then place the IUD into the uterus using a thin tube. The process can cause discomfort, cramping, or pain, particularly when the IUD passes through the cervix and is placed in the uterus.
While the level of pain varies from person to person, it’s normal to experience mild to moderate discomfort during the procedure. Fortunately, CDC IUD insertion pain management guidelines provide a variety of strategies to help reduce discomfort during and after insertion.
CDC IUD Insertion Pain Management: Key Recommendations
The CDC IUD insertion pain management guidelines suggest several approaches to managing pain and discomfort before, during, and after the procedure. These strategies can help make the process more tolerable, especially for women who are concerned about pain.
1. Pain Relievers
The CDC recommends taking over-the-counter pain relievers like ibuprofen or acetaminophen before the procedure to help manage pain. Ibuprofen is often preferred due to its anti-inflammatory properties, which can help reduce cramping. Your healthcare provider may suggest taking a dose about 30 to 60 minutes before the procedure.
2. Local Anesthetics
Some healthcare providers may use a local anesthetic to numb the cervix before inserting the IUD. This can help reduce the discomfort associated with passing the IUD through the cervical canal. The anesthetic may be applied as a gel or injected directly into the cervix.
3. Cervical Softening Agents
For women with a smaller or tighter cervix, especially those who have never given birth, healthcare providers may use cervical softening agents such as misoprostol. These medications help soften and open the cervix, making the insertion process smoother and less painful.
4. Distraction Techniques
Distraction techniques, such as listening to music or practicing deep breathing, can also help manage pain during IUD insertion. Some healthcare providers may encourage patients to focus on relaxation techniques or bring a friend or family member for support.
5. Post-Insertion Care
After the procedure, it’s common to experience cramping and light bleeding for a few days. The CDC recommends continuing to take over-the-counter pain relievers as needed, using heating pads to alleviate cramps, and avoiding strenuous activities for 24 hours.
Managing Pain After IUD Insertion
While some discomfort is expected after IUD insertion, severe or prolonged pain is not typical. Most women experience cramping similar to menstrual cramps for a few hours or days after the procedure, and this can be managed with pain relievers or other comfort measures.
If the pain persists or worsens, it’s important to consult with your healthcare provider. In rare cases, complications such as IUD expulsion or perforation can cause severe pain and require medical attention.
Benefits of an IUD Despite Pain Concerns
Despite concerns about pain during insertion, the long-term benefits of an IUD often outweigh the discomfort of the procedure. Here are some reasons why many women choose an IUD as their preferred method of contraception:
- Long-lasting protection: IUDs provide long-term birth control without the need for daily pills or regular injections. Depending on the type, an IUD can last anywhere from 3 to 10 years.
- Highly effective: IUDs are more than 99% effective at preventing pregnancy, making them one of the most reliable contraceptive options available.
- Reversible: IUDs can be removed at any time if you decide to become pregnant or switch to a different birth control method. Fertility typically returns quickly after removal.
- Hormonal and non-hormonal options: Women can choose between hormonal and copper IUDs, depending on their preferences and health needs.
- Minimal maintenance: Once inserted, an IUD requires little to no maintenance, providing worry-free protection for years.
FAQs About CDC IUD Insertion Pain Management
The level of pain during IUD insertion varies from person to person. Some women experience only mild discomfort, while others may feel moderate to severe cramping, especially when the IUD passes through the cervix. The CDC IUD insertion pain management guidelines recommend several strategies, including pain relievers and local anesthetics, to minimize discomfort.
Yes, it is recommended to take over-the-counter pain relievers like ibuprofen or acetaminophen about 30 to 60 minutes before the procedure. Ibuprofen is particularly helpful because it also reduces inflammation and cramping. Always follow your healthcare provider’s instructions for pre-procedure pain management.
Mild cramping and light bleeding are common for a few hours to days after IUD insertion. Over-the-counter pain relievers, heating pads, and rest can help manage post-insertion discomfort. If pain persists or worsens, contact your healthcare provider.
Most women tolerate IUDs well, but some may experience side effects such as irregular bleeding or cramping for the first few months after insertion. Serious complications, such as IUD expulsion or uterine perforation, are rare. It’s important to follow up with your healthcare provider if you experience any unusual symptoms.
If you’re concerned about pain during the procedure, talk to your healthcare provider. They can discuss CDC IUD insertion pain management options with you and help you decide if an IUD is the right choice for you. In some cases, using a local anesthetic, pain relievers, or cervical softeners can help reduce discomfort.
Conclusion
While IUD insertion can cause discomfort or pain for some women, there are several effective strategies for CDC IUD insertion pain management. With proper preparation and post-insertion care, many women find that the benefits of long-term, reliable contraception far outweigh the temporary discomfort of the procedure. If you’re considering an IUD, discuss pain management options with your healthcare provider to ensure a smooth and comfortable experience.
By understanding the CDC IUD insertion pain management recommendations and knowing what to expect, you can feel more confident and prepared for your IUD insertion process, making it a positive and manageable experience for your reproductive health.